Inguinal hernia
Inguinal Hernia
- Pain and tenderness in the area.
- Bulging in the groin
- Discomfort especially with coughing, exercise, or bowel movements.
- Weakness of the muscles & Ligaments of the abdomen.
- Constipation
- Straining at the time of urination and bowel movement
- More than 50 years or less than 1 year.
- Chronic cough
- Frequent sneezing
- Frequent heavy weight lifting
- Hard physical work
- Increased stress in the abdomen
- An old weak spot present in the abdominal wall
- Fluid in the abdomen or ascitis
- Premature birth
- Family history
- Smoking
- Chronic obstructive pulmonary disease (C.O.P.D.)
- Obesity
- Pregnancy
- Peritoneal Dialysis
- Collagen vascular disease
- Connective tissue disease
- Previous open appendectomy
- Based on symptoms
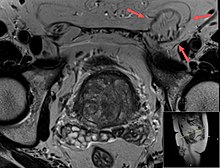
- C.T Scan : Imaging is used to confirm the diagnosis
- Ultrasound
- M.R.I
There are two types of inguinal hernia, direct and indirect, which are defined by their relationship to the inferior epigasric vessels. Direct inguinal hernias occur medial to the inferior epigastric vessels when abdominal contents herniate through a weak spot in the fascia of the posterior wall of the inguinal canal, which is formed by the transversalis fascia. Indirect inguinal hernias occur when abdominal contents protrude through the deep inguinal ring, lateral to the inferior epigastric vessels; this may be caused by failure of embryonic closure of the processus vaginalis.
In the case of the female, the opening of the superficial inguinal ring is smaller than that of the male. As a result, the possibility for hernias through the inguinal canal in males is much greater because they have a larger opening and therefore a much weaker wall through which the intestines may protrude.
Clinical classification of hernia is also important according to which hernia is classified into
- Reducible hernia: is one which can be pushed back into the abdomen by putting manual pressure to it.
- Irreducible/Incarcerated hernia: is one which cannot be pushed back into the abdomen by applying manual pressure.
Irreducible hernias are further classified into
- Obstructed hernia: is one in which the lumen of the herniated part of intestine is obstructed.
- Strangulated hernia: is one in which the blood supply of the hernia contents is cut off, thus, leading to ischemia. The lumen of the intestine may be patent or not.
The direct inguinal hernia enters through a weak point in the fascia of the abdominal wall and its sac is noted to be medial to the inferior epigastric vessels .Direct inguinal hernias may occur in males or females, but males are ten times more likely to get a direct inguinal hernia.
A direct inguinal hernia protrudes through a weakened area in the transversalis fascia near the medial inguinal fossa within an anatomic region known as the inguinal or Hesselbach's triangle, an area defined by the edge of the rectus abdominis muscle, the inguinal ligament and the inferior epigastric artery. These hernias are capable of exiting via the superficial inguinal ring and are unable to extend into the scrotum.
When a patient suffers a simultaneous direct and indirect hernia on the same side, the result is called a "pantaloon " hernia (because it looks like a pair of pants, with the epigastric vessels in the crotch), and the defects can be repaired separately or together.
Since the abdominal walls weaken with age, direct hernias tend to occur in the middle-aged and elderly. This is in contrast to indirect hernias which can occur at any age including the young, since their etiology includes a congenital component where the inguinal canal is left more patent (compared to individuals less susceptible to indirect hernias).
Indirect inguinal hernia
An indirect inguinal hernia results from the failure of embryonic closure of the deep inguinal ring after the testicle has passed through it. It is the most common cause of groin hernia.
In the male fetus, the peritoneum gives a coat to the testicle as it passes through this ring, forming a temporary connection called the processus vaginalis . In normal development, the processus is obliterated once the testicle is completely descended. The permanent coat of peritoneum that remains around the testicle is called the tunica vaginalis . The testicle remains connected to its blood vessels and the vas deferens, which make up the spermatic cord and descend through the inguinal canal to the scrotum.
The deep inguinal ring, which is the beginning of the inguinal canal, remains as an opening in the fascia transversalis, which forms the fascial inner wall of the spermatic cord. When the opening is larger than necessary for passage of the spermatic cord, the stage is set for an indirect inguinal hernia. The protrusion of peritoneum through the internal inguinal ring can be considered an incomplete obliteration of the processus.
In an indirect inguinal hernia, the protrusion passes through the deep inguinal ring and is located lateral to the inferior epigastric artery. Hence, the conjoint tendon is not weakened.
There are three main types
- Bubonocele: in this case the hernia is limited in inguinal canal.
- Funicular: here the processus vaginalis is closed at its lower end just above the epididymis. The content of the hernial sac can be felt separately from the testis which lies below the hernia.
- Complete (or scrotal): here the processus vaginalis is patent throughout. The hernial sac is continuous with the tunica vaginalis of the testis. The hernia descends down to the bottom of the scrotum and it is difficult to differentiate the testis from hernia.
In the female, groin hernias are only 4% as common as in males. Indirect inguinal hernia is still the most common groin hernia for females. If a woman has an indirect inguinal hernia, her internal inguinal ring is patent, which is abnormal for females. The protrusion of peritoneum is not called "processus vaginalis" in women, as this structure is related to the migration of the testicle to the scrotum. It is simply a hernia sac. The eventual destination of the hernia contents for a woman is the labium majus on the same side, and hernias can enlarge one labium dramatically if they are allowed to progress.
- Drink 3 glasses of water early in the morning.
- Take 1/2 teaspoon of Triphala powder with lukewarm water at night.
- Do not lift heavy weight.
- Treat chronic cough with antibiotics.
- Keep your weight in check.
- Do not Strain at the time of urination and bowel movement
- Keep your blood sugar in check.
- Avoid increased stress in the abdomen
- Quit smoking.
- Keep yourself hydrated.
- Eat high fiber diet : lots of salads, vegetables, fruits, sprouts.
- Eat multigrain flour (atta ) 10 kg wheat, 2 kg black gram 1 kg soyabean and 1 kg jao or barley.
- Eat pulses with cover (chilke vali dal)
- Conservative
- Surgery
Surgical
Surgical correction of inguinal hernias is called a hernia repair. It is not recommended in minimally symptomatic hernias, for which watchful waiting is advised, due to the risk of post herniorraphy pain syndrome. Surgery is commonly performed as outpatient surgery. There are various surgical strategies which may be considered in the planning of inguinal hernia repair. These include the consideration of mesh use (e.g. synthetic or biologic ), open repair, use of laparoscopy, type of anesthesia (general or local), appropriateness of bilateral repair, etc. Laparoscopy is most commonly used for non-emergency cases, however, a minimally invasive open repair may have a lower incidence of post-operative nausea and mesh associated pain. During surgery conducted under local anesthesia, the patient will be asked to cough and strain during the procedure to help in demonstrating that the repair is without tension and sound.
Constipation after hernia repair results in strain to evacuate the bowel causing pain, and fear that the sutures may rupture. Opioid analgesia makes constipation worse. Promoting an easy bowel motion is important post-operatively.
Surgical correction is always recommended for inguinal hernias in children.
Emergency surgery for incarceration and strangulation carry much higher risk than planned, "elective" procedures. However, the risk of incarceration is low, evaluated at 0.2% per year. On the other hand, surgery has a risk of inguinodynia (10-12%), and this is why males with minimal symptoms are advised to watchful waiting. However, if they experience discomfort while doing physical activities or they routinely avoid them for fear of pain, they should seek surgical evaluation. For female patients, surgery is recommended even for asymptomatic patients.














Comments
Post a Comment