Osteoporosis (Porous Bone disease, Asthi Soushirya)
Osteoporosis
(Fragility Fracture / Porous Bone disease, Fragile bone tissue. Asthi Soushirya, अस्थि क्षय)Osteoporosis is a bone disease that occurs when the body loses too much bone, makes too little bone, or both. As a result, bones become weak and may break from a fall or, in serious cases, from sneezing or minor bumps. Osteoporosis means “porous bone.” Did you know that calcium keeps you looking young and beautiful. Here's how? Like many women, you may know that the minimum daily calcium requirement is 1,000 milligrams (mg) for women of 50 and younger and 1,200 mg for women over 50. Adequate calcium is necessary for good health, and not just because it's a major component of our bones. It also plays a vital role in keeping our organs and skeletal muscles working properly. The body gets the calcium it needs for basic functions by releasing the calcium stores in our bones into the blood through bone remodeling - the process by which bone is constantly broken down and rebuilt. If your body doesn't get enough calcium, it takes it from your bones making them weak and putting you at risk of osteoporosis.
"BONE IS A LIVING TISSUE THAT IS COSTANTLY BEING BROKEN DOWN AND REPLACED."
Calcium plays a major role in providing firmness and elasticity to the skin as well as all the tissues and cells of the body- helping you stay strong and look beautiful. Calcium rich food can also deter acne. Calcium is essential in building bone. Calcium is a mineral that is necessary for life. In addition to building bones and keeping them healthy, calcium enables our blood to clot, our muscles to contract and our heart to beat. About 90% of calcium in our bodies is in our bones and teeth.
Every day we lose calcium through our skin, nails, hair, sweat, urine & feces. Our bodies cannot produce its own calcium. That's why it's important to get enough calcium from the food we eat. When we don't get the calcium our body needs, it is taken from our bones. This is fine once in a while, but if it happens too often, bone get week and easier to break. It all eventually lead to bone loss, low bone density and even broken bones.
- Vitamin D helps the body in calcium absorption and augments bone health. When the body is exposed to sunlight, it converts cholesterol into vitamin D. Therefore the easiest cure for osteoporosis is generous exposure of the body to the Sunlight for 30 minutes every day.
Calcium Deficiency
- Post - menopausal Bone loss increases after the menopause due to lower levels of estrogen, and after Andropause due to lower levels of Testosterones
- Heredity If a person is having history of osteoporosis then he/she is more suspicious to get affected.
- Drugs Prolonged use of steroids ( in Asthma) and some medicines such as anti-convulsant , lead to osteoporosis.
- Immobilization Prolonged bed rest and total lack of activity , specially in elders.
- Gender Females are more prone than males. In males the bone cell components and the structure of bone cells is harder, firm in make, compared to females. after delivery, the calcium level in female gets reduced.
- Nutritional a) Altered and insufficient diet. b) Poor calcium intake. c) Poor calcium absorption.
- Low body weight/ body’s inability to absorb and utilize nutrients
- Prolonged deficiency of calcium and vitamin D
- Sedentary lifestyle/ unhealthy diet
- Smoking/ chronic alcoholism
- Crash dieting/ nutritional deficiency
- Elderly Aged people are likely to get osteoporosis as a degenerative change.
- Inadequate sunlight exposure
- Disease like Alcoholism, Hyperthyroidism, anorexia, Kidney diseases.
- Surgical removal of ovaries.
- Medications like antiseizure, chemotherapy, glucocorticosteroids.
- According to Ayurveda, it is considered as a metabolic disorder related to the formation of bones. As osteoporosis is a Vata/ Kapha predominant disease. The "Gramyahara" i.e. improper diet leads to the deformities in bones and muscles. Excessive salty, spicy, fermented food alters the production of Asthi (bones). The food which contains preservatives; alkaline substances if consumed more, destroys the bone tissues and increases its porosity. On the contrary the smooth, oily; soft, sweet and nutritious food helps in prevention of porosity. Intake of toxic substances like tobacco, cigarettes , alcohol and coffee also increases porosity .
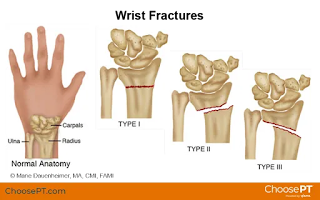
- Fractures are common symptoms of osteoporosis and can result in disability.
- Pain : Acute and chronic pain in the elderly due to osteoporosis.
- Sudden back pain
- Tiredness
- Hunchback, A gradual loss of height
- Lame : Severe pain in elderly patient i.e. joints, bones and limb
- Rounding off the shoulders
- Gum inflammation, Falling of teeth
 |
| Gum disease |
- Acute lower backache/ spasms of back muscles
- Swelling of a wrist, after a minor fall or injury
- Constant trouble with nails, hair, teeth, gums, joints, or back
- Nocturnal leg cramps/spinal disc collapse
- Bone degeneration :Compound fracture after a simple fall
- Aching of long bones/ thinning of pelvic bone/feeling of emptiness of bones.
- Loss of twisting and bending strength
- Frequent occurrence of spontaneous fracture
- Numbness, tingling fingers, muscles cramps, lethargy poor appetite, weak or brittle finger nails, dry skin.
- Weakness of bone, loss of elasticity of joints
- Insomnia, vertigo, blackouts.
- Looseness of major joints
- Loosening of teeth, Falling of hairs, and eye lashes.
- Dry skin : Due to vata vitiation
 |
| Dry skin |
- Cracking of teeth.
- Dryness of mouth
- Anemic condition. Emaciation of muscle
- Emaciation of muscles
Fractures of the long bones acutely impair mobility and may require surgery. hip fracture, in particular, usually requires prompt surgery, as serious risks are associated with it, such as deep vein thrombosis and pulmonary embolism, and increased mortality.
Fracture risk calculators assess the risk of fracture based upon several criteria, including bone mineral density, age, smoking, alcohol usage, weight, and gender.
The term "established osteoporosis" is used when a broken bone due to osteoporosis has occurred. Osteoporosis is a part of fragility syndrome.
.jpg) |
| Progression of the shape of vertebral column with age in Osteoporosis |
Osteoporosis Location
The underlying mechanism in all cases of osteoporosis is an imbalance between bone absorption and bone formation In normal bone, matrix remodeling of bone is constant; up to 10% of all bone mass may be undergoing remodeling at any point in time. Osteoclasts are assisted by transcription factor PU.1 to degrade the bone matrix, while osteoblast rebuild the bone matrix. Low bone mass density can then occur when osteoclasts are degrading the bone matrix faster than the osteoblasts are rebuilding the bone.
The three main mechanisms by which osteoporosis develops are an inadequate peak bone mass (the skeleton develops insufficient mass and strength during growth), excessive bone resorption, and inadequate formation of new bone during remodeling, likely due to mesenchymal stem cells biasing away from the osteoblast and toward the marrow adipocyte lineage. An interplay of these three mechanisms underlies the development of fragile bone tissue. Hormonal factors strongly determine the rate of bone resorption; lack of estrogen (e.g. as a result of menopause) increases bone resorption, as well as decreasing the deposition of new bone that normally takes place in weight-bearing bones. The amount of estrogen needed to suppress this process is lower than that normally needed to stimulate the uterus and breast gland . The α-form of the estrogen receptor appears to be the most important in regulating bone turnover. In addition to estrogen, calcium metabolism plays a significant role in bone turnover, and deficiency of calcium and vitamin D leads to impaired bone deposition; in addition, the parathyroid glands react to low calcium levels by secreting parathyroid hormone (parathormone, PTH), which increases bone resorption to ensure sufficient calcium in the blood. The role of calcitonin, a hormone generated by the thyroid that increases bone deposition.

Collapse of vertebra on right, normal on left due to fracture
"All women 65 years of age or older be screened by Bone densitometry and screening younger women with risk, BMD testing for men 70 or older.".

Diagnosis
- History of fracture
- X - Ray : The diagnosis of osteoporosis can be made using conventional radiography
- By measuring Bone Mineral Density : : Bone Mineral Density Scan Osteoporosis is defined as a bone density of 2.5 standard deviation below that of a young adult. This is typically measured by dual-energy X-ray absorptiometry (DEXA Scanner). It measures bone mineral density (BMD) using spectral imaging. Two X- ray beams with different energy levels, are aimed at patient's bones. When soft tissue absorption is subtracted out the BMD can be determined from the absorption of each beam by bone. The DXA scan is typically used to diagnose and follow osteoporosis, as contrasted to the nuclear bone scan, which is sensitive to certain metabolic diseases of bones in which bones are attempting to heal from infections, fractures, or tumors. It is also sometimes used to assess bone composition.
 |
| DXA / DEXA Scanner |
Dual - energy X- Ray absorptiometry (DEXA scan) is considered the gold standard for the diagnosis of osteoporosis. Osteoporosis is diagnosed when the bone mineral density is less than or equal to 2.5 standard deviations below that of a young (30–40-year-old), healthy adult women reference population. This is translated as a T - score . But because bone density decreases with age, more people become osteoporotic with increasing age. The World Health Organization has established the following diagnostic guidelines:
| Category | T-score range | % young women |
|---|---|---|
| Normal | T-score ≥ −1.0 | 85% |
| Osteopenia | −2.5 < T-score < −1.0 | 14% |
| Osteoporosis | T-score ≤ −2.5 | 0.6% |
| Severe osteoporosis | T-score ≤ −2.5 with fragility fracture |
Quantitative Ultrasound
Quantitative ultrasound has many advantages in assessing osteoporosis. The modality is small, no ionizing radiation is involved, measurements can be made quickly and easily, and the cost of the device is low compared with DXA and QCT devices. The calcaneus is the most common skeletal site for quantitative ultrasound assessment because it has a high percentage of trabecular bone that is replaced more often than cortical bone, providing early evidence of metabolic change. Also, the calcaneus is fairly flat and parallel, reducing repositioning errors. The method can be applied to children, neonates, and preterm infants, just as well as to adults. Some ultrasound devices can be used on the tibia..jpg)
Tibia
.jpg)
Biomarkers
Chemical biomarkers are a useful tool in detecting bone degradation. The enzyme cathepsin K breaks down Type -1 collagen, an important constituent in bones. Prepared antibodies can recognize the resulting fragment, called a neoepitope, as a way to diagnose osteoporosis. Increased urinary excretion of C-telopeptides, a type-I collagen breakdown product, also serves as a biomarker for osteoporosis.
- Osteoporosis is perfectly diagnosed with the help of bone density measurement machine
- Bone mass measurement
- Dual photon absorptiometry (DPA)
- Dual energy X-ray absorptiometry (DEXA) are used to measure the bone mass of spine and femoral neck.
- CT or MRI scan
Fracture risk assessment
In the absence of risk factors other than sex and age a BMD measurement using dual-energy X-ray absorptiometry (DXA) is recommended for women at age 65. For women with risk factors a clinical FRAX is advised at age 50.
Risk of fall
Complication
Depression is considered to a complication of osteoporosis. People with osteoporosis lose independence and risk being isolated due to less physical activity. This will further hinder the ability to manage health issues.
Osteoporosis is also linked to respiratory and cardiovascular health issues, such as loss of lung capacity. Multiple fractures lead to a collapsed thoracic spine, which makes less air being able to move into the lungs. Every thoracic vertebral body collapsed results in the loss of nearly 10% of lung volume.
Risk Factors
Non Modifiable
- The most important risk factors for osteoporosis are advanced age (in both men and women) and female sex; estrogen deficiency following menopause or surgical removal of ovaries is correlated with a rapid reduction in bone mineral density, while in men, a decrease in testosterone levels has a comparable (but less pronounced) effect.
- Ethnicity: While osteoporosis occurs in people from all ethnic groups, European or Asian ancestry predisposes for osteoporosis.
- Heredity: Those with a family history of fracture or osteoporosis are at an increased risk; the heritability of the fracture, as well as low bone mineral density, is relatively high, ranging from 25 to 80%. At least 30 genes are associated with the development of osteoporosis.
- Those who have already had a fracture are at least twice as likely to have another fracture compared to someone of the same age and sex.
- Build: A small stature is also a nonmodifiable risk factor associated with the development of osteoporosis.
- Excessive alcohol: Chronic heavy drinking (alcohol intake greater than three units/day) probably increases fracture risk despite any beneficial effects on bone density.
- Vitamin D deficiency : Low circulating Vitamin D is common among the elderly worldwide. Mild vitamin D insufficiency is associated with increased parathyroid hormone (PTH) production. PTH increases bone resorption, leading to bone loss. A positive association exists between serum 1,25-dihydroxycholecalciferol levels and bone mineral density, while PTH is negatively associated with bone mineral density.
- Tobacco Smoking : Tobacco smoking has been proposed to inhibit the activity of osteoblasts, and is an independent risk factor for osteoporosis. Smoking also results in increased breakdown of exogenous estrogen, lower body weight and earlier menopause, all of which contribute to lower bone mineral density.
- Malnutrition : Nutrition has an important and complex role in maintenance of good bone. Identified risk factors include low dietary calcium and/or phosphorus, magnesium, zinc, boron, iron, fluoride, copper, vitamins A, K, E and C (and D where skin exposure to sunlight provides an inadequate supply). Excess sodium is a risk factor. High blood acidity may be diet-related, and is a known antagonist
- A diet high in protein may be optimal for bone health, as higher protein diets tend to increase absorption of calcium from the diet and are associated with higher bone density.
- Underweight/ inactive : Bone remodeling occurs in response to physical stress, so physical inactivity can lead to significant bone loss. Weight bearing exercise can increase peak bone mass achieved in adolescence, and a highly significant correlation between bone strength and muscle strength has been determined. The incidence of osteoporosis is lower in overweight people.
- Endurance training: In female endurance athletes, large volumes of training can lead to decreased bone density and an increased risk of osteoporosis. This effect might be caused by intense training suppressing menstruation, producing amenorrhea, and it is part of the female athlete traid. However, for male athletes, the situation is less clear, and although some studies have reported low bone density in elite male endurance athletes, others have instead seen increased leg bone density.
- Heavy metals : A strong association between cadmium and lead with bone disease has been established. Low-level exposure to cadmium is associated with an increased loss of bone mineral density readily in both genders, leading to pain and increased risk of fractures, especially in the elderly and in females. Higher cadmium exposure results in osteomalacia (softening of the bone)
- Soft drinks: Soft drinks (many of which contain phosphoric acid ) may increase risk of osteoporosis, at least in women.
- Proton pump inhibitors (such as lansoprazole, esomeprazole, and omeprazole), which decrease the production of stomach acid are a risk factor for bone fractures if taken for two or more years, due to decreased absorption of calcium in the stomach.
- In general, immobilization causes bone loss (following the 'use it or lose it' rule). For example, localized osteoporosis can occur after prolonged immobilization of a fractured limb in a cast. This is also more common in active people with a high bone turn-over (for example, athletes). Other examples include bone loss during space flight or in people who are bedridden or use wheelchairs for various reasons.
- Hypogonadal states can cause secondary osteoporosis. These include Turners syndrome, Klinefelter syndrome, anorexia nervosa, andropause, hypothalamic or amenorrhea or hyperprolactemia. In females, the effect of hypogonadism is mediated by estrogen deficiency. It can appear as early menopause (<45 years) or from prolonged premenopausal amenorrhea (>1 year). Bilateral oophorectomy (surgical removal of the ovaries) and premature ovarian failure cause deficient estrogen production. In males, testosterone deficiency is the cause (for example, andropause or after surgical removal of the testes).
- Endocrine disorders that can induce bone loss include, Cushing's syndrome, hyper parathyroids, hyperthyroidism, diabetes mellitus, type 1 and 2, acromegaly and adrenal insufficiency.
- Malnutrition, parenteral nutrition and malabsorption can lead to osteoporosis. Nutritional and gastrointestinal disorders that can predispose to osteoporosis include undiagnosed and untreated coeliac disease (both symptomatic and asymptomatic people), Crohn's disease, ulcerative colitis, cystic fibrosis, surgery (after gastrectomy, intestinal bypass surgery or bowel resection ) and severe liver diseases (especially primary biliary cirrhosis ). People with lactose intolerance or milk allergy may develop osteoporosis due to restrictions of calcium-containing foods. Individuals with bulimia can also develop osteoporosis. Those with an otherwise adequate calcium intake can develop osteoporosis due to the inability to absorb calcium and/or vitamin D. Other micronutrients such as vitamin K, or vitamin B12 deficiency may also contribute.
- People with rheumatologic disorders such as rheumatoid arthritis, ankylosing spondylosis, systemic lupus erythematosus and polyarticular juvenile idiopathic arthritis are at increased risk of osteoporosis, either as part of their disease or because of other risk factors (notably corticosteroid therapy). Systemic diseases such as amyloidosis and sarcoidosis can also lead to osteoporosis.
- Chronic kidney disease can lead to renal osteodystrophy
- Hematologic disorders linked to osteoporosis are multiple myeloma and other monoclonal gammopathies, lymphoma, leukemia, mastocytosis, hemophilia,, sickle disease and thalassemia.
- Several inherited or genetic disorders have been linked to osteoporosis. These include osteogenesis, imperfecta, Multicentric carpotarsal osteolysis syndrome, Multicentric osteolysis, Nodulosis, and arthropathy. Marfan syndrome, hemochromatosis, hypophosphatasia, (for which it is often misdiagnosed),
- People with scoliosis of unknown cause also have a higher risk of osteoporosis. Bone loss can be a feature of complex regional pain syndrome. It is also more frequent in people with Parkinson's disease and chronic obstructive pulmonary disease.
- People with Parkinson's disease have a higher risk of broken bones. This is related to poor balance and poor bone density. In Parkinson's disease there may be a link between the loss of dopaminergic neurons and altered calcium metabolism (and iron metabolism) causing a stiffening of the skeleton and kyphosis.
Medication
Certain medications have been associated with an increase in osteoporosis risk; only glucocorticosteroids and anticonvulsants are classically associated, but evidence is emerging with regard to other drugs.
- Steroid induced osteoporosis (SIOP) arises due to use of glucocorticoids – analogous to Cushing's syndrome and involving mainly the axial skeleton. The synthetic glucocorticoid prescription drug prednisone is a main candidate after prolonged intake. Some professional guidelines recommend prophylaxis in patients who take the equivalent of more than 30 mg hydrocortisone (7.5 mg of prednisolone), especially when this is in excess of three months. It is recommended to use calcium or Vitamin D as prevention. Alternate day use may not prevent this complication.
- Barbiturates phenytoin and some other enzyme-inducing antiepileptics – these probably accelerate the metabolism of vitamin D.
- L-Thyroxine over-replacement may contribute to osteoporosis, in a similar fashion as thyrotoxicosis does. This can be relevant in subclinical hypothyroidism.
- Several drugs induce hypogonadism, for example aromatase inhibitors used in breast cancer, methotrexate and other antimetabolite drugs, depo progesterone and gonadotropin releasing hormone agonists.
- Anticoagulants – long-term use of heparin is associated with a decrease in bone density, and warfarin (and related coumarins) have been linked with an increased risk in osteoporotic fracture in long-term use.
- Proton pump inhibitor – these drugs inhibit the production of stomach acid ; this is thought to interfere with calcium absorption. Chronic phosphate binding may also occur with aluminum -containing antacids.
- Thiazolidinediones (used for diabetes) – rosiglitazone and possibly pioglitazone, inhibitors of PPARy, have been linked with an increased risk of osteoporosis and fracture.
- Chronic lithium therapy has been associated with osteoporosis.
Differential Diagnosis
- Costochondritis (kos-toe-kon-DRY-tis) is an inflammation of the cartilage that connects a rib to the breastbone (sternum). Pain caused by costochondritis might mimic that of a heart attack or other heart conditions. Over-the-counter nonsteroidal anti-inflammatory drugs
- Occurs on the left side of your breastbone, Is sharp, aching or pressure-like, Affects more than one rib, Worsens when you take a deep breath or cough.
- While there is no laboratory or imaging test to confirm a diagnosis of costochondritis
- Treatment : Stretching exercises and Pain relievers. Ask your doctor about using ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve, others). Heat or ice. Try placing hot compresses or a heating pad on the painful area several times a day. Rest.
Lifestyle
- Plenty of sunshine. Sunlight is the best source of vitamin D. There should be half an hour sunlight exposure every day for strong bones.
- Nutritious diet with calcium supplement at least 1 gram daily.
- Before 21 years of age take good care of your bones
- Keep your digestive system healthy
- One should eat slowly and chew the food extremely well
- The essential vitamin-D directly influences the absorption of calcium and phosphorus compounds from the intestine.
- Measuring 400 I U of Vitamin D is recommended.
- A cup of milk daily helps in meeting the calcium requirement of the body and thus helps in building strong bones.
- One boiled egg a day also can lead to strong bones in a growing child.
- Low stress/ proper breathing/ spend time outdoor;
- Bisphosphonate medications are useful to decrease future broken bones in those with previous broken bones due to osteoporosis.
- Routine like head rotation/ shoulder movement/ movement of other joints
- Removal of carpets or other items facilitating falls.
- Wear well fitted footwears.
- Proper diet during childhood.
- Modify habits (laced shoes, illuminate house at night, install railings, non-skid tiles in bathroom).
- Removal of obstacles and loose carpets in the living environment may substantially reduce falls.
- Avoid spilling water on floor while mopping the floor.
- In people with coeliac disease adherence to gluten free diet decreases the risk of osteoporosis and increase bone density.
- Efforts to avoid medications that increases the rate of bone loss.
- Exercise daily : Walking + light weight. There is some evidence that physical exercise may be beneficial for bone density in postmenopausal women and lead to a slightly reduced risk of a bone fracture.
- A increased bone activity and weight-bearing exercises at a young age prevent bone fragility in adults.
- No Tobacco smoking.
- Abstinence from alcohol,
- Fall prevention can help prevent osteoporosis complications
- Plenty of sunshine. Sunlight is the best source of vitamin D. There should be half an hour sunlight exposure every day for strong bones.
For Senior Citizens
Yoga
To learn to squat or if you are pregnant: Separate your feet about 6 to 8 inches, and place a folded blanket under your heels until you are able to lower your pelvis and maintain balance.
- This asana strengthens abdominal and pelvic muscles, increases blood circulation and aids in digestion.
"However, one need not become slave of one's desire."
Squatting

Awareness on synchronization of breath with body movement, maintaining balance and stretch of the whole body.
Benefit :
- It strengthens knee, thigh and ankle.
- Strengthens the body
- Relaxes the muscles
- Improves the posture
- Enhances body flexibility
- Increases height in formative years.
- Boost mental awareness
- Promotes weight loss.
- Boosts Energy Levels.
- Improves Your Mood.
- Provides Relief From Sciatica.
Benefit :
- Improves balance and stability in the legs.
- On a metaphysical level, helps one to achieve balance in other aspects of life.
- Strengthens the ligaments and tendon of the feet.
- Strengthens and tones the entire standing leg, up to the buttocks.
- Assists the body in establishing pelvic stability.
---------------------------------------------------------------------------------------------------------------
: In this, stand back to a wall and separate the feet. Now walk the left foot about a couple of inches, while maintaining your balance. Now, stretch the arms horizontally while turning the right foot perpendicular to the left. Maintain the arm in an outstretched position and breathe for about half a minute. Straightened up and do the same for opposite side.
Benefit :
- Stretches and strengthens the thighs, knees, and ankles.
- Stretches the hips, groins, hamstrings, and calves; shoulders, chest, and spine.
- Stimulates the abdominal organs.
- Helps relieve stress.
- Improves digestion.
- Helps relieve the symptoms of menopause.
Benefit:
- Strengthens your shoulders, arms, legs, ankles and back.
- Opens yours hips, chest and lungs.
- Improves focus, balance and stability.
- Encourages good circulation and respiration.
- Stretches your arms, legs, shoulders, neck, belly, groins and ankles.
- Energizes the entire body.
- Reduces fat on thighs.
- Opens up the hips, stretching deep hip flexors.
- Stretches and strengthens the shoulders and back.
- Expands the abdominal region, improving digestion and elimination.
- Improves posture.
- Opens the chest, improving respiration.
- Loosens up the vertebrae.
- Relieves lower back pain.
- Relieves stress on your neck muscle but also helps to make your back supple.
Benefit :
- Stronger arms legs, knees and ankles.
- Open shoulder joints, creating space between the shoulder blades'
- Open hips and IT band
- Increased circulation to all joints.
- Improved digestion and elimination.
- Improved balance
- Improved focus.
● Dogs Pose Adho Mukha Svanasana (अधो मुख स्वानासन )

Technique : Come down on all fours. Keep your back extremely straight. Come into your fours. Form a table such that your back forms a table top and your hands and feet form the legs of the table. As you breathe out to lift the hips up, straightening the knees and elbows, form an inverted V–shape with the body. Hands are shoulder width apart, feet are hip width apart and parallel to each other, toes point straight ahead. Press your hands into the ground wide through the shoulder blades. Keep the neck lengthened by touching the ears to the inner arms. Hold the downward dog pose and take long deep breaths. Look towards the naval. Exhale bends the knees, return to table pose, Relax.
- Calms the brain and helps relieve stress and mild depression.
- Energizes the body.
- Stretches the shoulders, hamstrings, calves, arches, and hands.
- Strengthens the arms and legs.
- Helps relieve the symptoms of menopause.
- Relieves menstrual discomfort when done with head supported.
- Helps prevent osteoporosis
How to do it?
Step 1: Lie down on the back.
Step 2: Inhale and place the palms on the floor beside the head with the fingers pointing towards the shoulders, and the knees bent and heels touching the buttocks.
Step 3: Retain the breath and then slowly lift the trunk from the floor.
Step 4: With normal breathing, slowly lift the back and the trunk and give weight to the palm.
Step 5: Create an arch with normal breathing and hold the final position for as long as comfortable.
Step 6: At the last step, Exhale and slowly lower the body so the head rests on the floor and then lower the rest of the body.
- Good for first chakra.
- An inter medial yoga pose that open in front of all the Chakras.
- Stretches the chest and lungs.
- Strengthens the arms and wrists, legs, buttocks, abdomen, and spine.
- Stimulates the thyroid and pituitary.
- Increases energy and counteracts depression.
- Therapeutic for asthma, back pain, infertility, and osteoporosis.
Contra-indication
1) People who have weak wrist or unable to support the whole body by their arms should refrain from doing this.
2) People suffering from frequent headaches and migraine should avoid doing it.
3) People suffering from spinal ailments like cervical and lumbar spondylitis should not do this.
4) It is not supportable to the people who have stomach ulcers, heart problems and High Blood Pressure.
5) If anyone feeling dizziness then it should not be done.
6) It is not recommended to a diabetic patient.
7) People having acidity should avoid Chakrasana.
- The posture is a panacea for an injured spine and in cases if slight displacement of spinal discs.
- The practice of this pose replace the discs in their original position
- The spinal region is fully toned and the chest fully expanded.
- This asana is beneficial in diabetes, bronchitis, asthma and spondylitis.
- This asana is very useful in relieving stiffness in upper back and also boost flexibility in lower back while strengthening our core muscles
- Opens up the shoulders and neck.
- Tones the abdomen.
- Strengthens the entire back and shoulders.
- Improves flexibility of the upper and middle back.
- Expands the chest.
- Improves blood circulation.
- Reduces fatigue and stress.
- Useful for people with respiratory disorders such as asthma. (Do not practice this yoga pose during the attack though).
- Flexibility of the dorsal spine, strengthens the spinal muscles. Prevent back pain. Reduces abdominal fat.
Pranayama
- Anolom Vilom Alternate nostril breathing- This is a calming and powerful pranayama
- Kapalabhati (Skull Shining breathing technique)- Normal inspiration and forceful expiration.
- Omkar Meditation- Chanting “OM” is a powerful way to control your nerves. It can be practiced at bedtime.
- Bhramari (Bee breathing)- The vibrations generated by this bee breath pranayama resonate within a deeply relaxing body and mind.
Exercises
- Sit To Stand Maneuver
Sit up tall in a sturdy chair (that won't slide) with your feet shoulder wide apart ; move forward to the front of the chair ; place your feet so that your heels are slightly behind your knees. Hinge forward from the hips, keeping the spine long, and place your hands on your thighs, stand up, putting equal weight through both legs. Sit down by hinging at the hips and lowering your self with control. Keep up your chest throughout the exercise. Repeat 10 times. To further challenge yourself, you can place your arm across your chest or use a shorter chair or hold light weight in your hands while doing the exercise.
- Weight-bearing exercises like sitting on the chair without chair/ running/ jumping/ lifting/ jogging
 |
| Best Bone Strengthening workout Resistance Exercises |
- Playing outdoor games/climbing staircase
- Walking for half an hour daily
- Cycling, swimming, dancing
- Spinal extension exercises
- Physical exercise and maintenance of muscular strength in the elderly (walking, swimming)
- This mudra is beneficial in any bone related disease, as the calcium content within the body increases.
- This mudra removes tooth problems and makes the teeth strong.
Marma
- Manibandha Marma- It is located at the wrist joint, holding the wrist of one hand with the middle finger and thumb of another hand on the dorsal side stimulates it. Then rotate your hand in clockwise and anti-clockwise direction. It should be done for 15-18 times.
- Kukundara marma It is located at the back, where the pelvic girdle and the vertebral column meet, at the region of a belt, two in number. Stimulation- Sit in vajrasana or sukhasana, keep your hand over belt line with the help of thumb press sacroiliac joint 15-18 times.
- Katika taruna marma It is situated at the back at the location of sciatic notch. Stimulation- Sit in vajrasana buttocks resting on the heels.
Chakra
Diet
- Edamame : Edamame is a Japanese dish prepared with immature soybeans in the pod. The pods are boiled or steamed and may be served with salt or other condiments. The dish has become popular across the world because it is rich in vitamins, dietary fiber, and isoflavones.
- of natural levels of phytoestrogens. Specially eaten in Japan.
-
- Vitamin D and Calcium rich in foods for healthy bones: Fresh fruit salad :
- Drumstick leaves : Moringa (Drumstick) has much more calcium found in milk which builds strong bones and teeth. It helps prevents osteoporosis.
- Eat wholesome food
- Dairy products : milk, ghee, buttermilk, yogurt, are ideal for building bone tissue.
- Home made cottage cheese
- Ground Nuts- 100 gm / day
- Oat Dalia, bajra khichri, bajra roti
- Sesame seed (til)- laddoo, rewadi, chatani, chikki
- Sunflower seeds are excellent food for osteoporosis
- Jaggery- 50 gms/ day and Kala Chana
- Fenugreek- seeds, laddoo, vegetable
- Sprouts moong, moth (mataki)
- Mixed grain bread, Missi roti
- Salad Beetroot, carrot, celery, cabbage
- Soup tomato, meat, ragi, vegetable, moong dal
- Betal leaves, curry leaves
- Supari (Areca catechu) 10 gms per week
- Egg- 1 per day (yolk), vitamin D supplement
- Fish- 200 GMs /day
- Mushrooms- 150 gms / month
- Raw juices fruits and vegetable orange, lemon pineapple, Papaya green leafy vegetables beetroot, carrot
- Soybeans in form of soya milk, tofu
- Eating 1 tsp Amla powder daily, Amla Murabba, Chyawanprash, Amla candy
- Cereals like oat, bajra, wheat
- Roasted flax seed and till tsp daily
- Almond, plum, figs
- Vegetables such as green leafy vegetables, snake gourd, broccoli, garlic, parwal, Chauli (Amaranthus ) turnips, cabbage, tomato, ridge gourd
- Drumstick leaves (8-10), flower and fruit
- Fruits such as guava, strawberries, avocado, pomegranate, grapes
- Pith and flower of plantain (banana)
- Seafood such as salmon and sardines
- Conch shell
- Millet such as ragi, Quinoa Asparagus
- Pulses : Dilochus biflorus or horse gram is known as (kulath dal) in Hindi. Its high in calcium, iron and proteins.
a) Nutritious Roti - Ground flour of raw bananas, Soozi ( Rava) , rice flour + cumin seeds+ garlic + chilly ; little salt should be served with home made butter.
b) Nutritious Dosa Rice flour, gram flour, Shingada flour (water chestnut) Methi, buttermilk, chilly , salt. Make dosa of this flour and serve hot with chutney of fresh coconut.
c) Puri Wheat flour, gram flour, soozi, chilly, salt. Fry this in ghee.
d) Solakari ( Sour soup of Vrikshmla) Crush fresh coconut and prepare coconut milk. add Kokum juice (Garcinia indica) black pepper ,saindhav salt and chilly.
f) Tomato soup Make a soup of coconut milk and tomato puree.
g) Upma Make upma of Dalia ( prepared from wheat)
g) Gram soup Make a soup of gram flour, grated coconut, Owa, ( ajwain) and salt. As gram ,wheat ; coconut are nutritious and avoid the degenerative changes.
f) Kulath Dal Pulses : Dilochus biflorus or horse gram is known as (kulath dal) in Hindi. Its high in calcium, iron and proteins.
1 Laddu Dink Laddu: Laddu prepared from "Gum acacia" , the nutritious resin.
2 Shira Shira prepared from Badam, green gram, Banana and fresh coconut.
3 Kheer a Wheat flour, coconut, dry fruits b) Rice Kheer c) Rice prepared from Shingada flour.
4 Sweet Uttappa a) Rice Uttappa - Uttappa made up from Rice flour, milk, sugar, mango juice processed in ghee. b) Wheat Uttappa - Wheat flour , milk and sugar.
5 Petha The sweet made up from Ash gourd (Benincasa cerifera). Other sweets prepared from coconut and milk.
6 Fruits Fresh fruits like Jack fruit, mango ,and banana.
7 Vegetables Vegetables of Raw Banana and raw Jack fruit.
B Non Vegetarian Diet
Paya Soup Bone soup
Nali Shorba Mogalai soup - Bone soup.
Nali Nahari Mutton soup.
Mutton Paya.
Egg Omlette processed in ghee.
- Late meals and overeating
- Avoid corticosteroid, chronic use of steroids is associated with secondary osteoporosis and fractures.
- Avoid tea, coffee, white sugar, white flour products
- Processed refined denatured food
- Smoking, alcohol
- Avoid the diet which increases Vayu.
Herbs
- Ginger
- Long pepper
- Cinnamon
- Phytoestrogens herbs used to help postmenopausal women Alfalfa, parsley, sage, aniseed, fennel, liquorice
- Incompatible diet - Food like consumption of milk and fish together.
- Excessive use if salty, spicy and hot food.
- Excessive use of fermented food like bread.
- Food with Preservatives.
- Food which is alkaline and penetrating.
- Stale and dry food.
- Pop a handful of sesame seeds (til) seeds every morning, an effective home remedy for osteoporosis, sesame seeds provides 1,000 mg of natural calcium in a handful (til laddoo).
- Almond milk is another good home remedy to cure osteoporosis, it is a rich source of calcium which is required for healthy bones. You can easily make it at home by soaking almonds in warm water, peeling, grinding and mixing with milk.
- Another cure for osteoporosis is consuming soy products. Since imbalance of hormone results in bone loss, soy product helps in balancing the estrogen level required for women suffering from osteoporosis.
- Manganese is a vital mineral for treating osteoporosis according to the latest studies. Manganese rich food such as pineapple, spinach, beans, nuts and whole wheat in the diet.
- A little bit of ragi added to wheat flour of chapattis daily can do wonders for the bones in just a few months.
 |
| Drumstick |
- Bone Broth : It contain high amount of collagen, which is ideal for cell growth. Also it is high on protein and low on calories, making it ideal for weight loss. Bone broth keeps one satiated for long, keep the body hydrated and improves skin and hairs and nails too,
Treatment
- Sodium alendronate 10mg/d or 70mg once a week.
- Risedronate 5mg/dose or 30mg once a week
- Ibandronate 150mg once a month
- If patient cannot tolerate bisphosphonates or mostly used in patients with established osteoporosis 250 mcg/ml, injection once daily.
- 2g oral suspension daily.
- In Hypogonadal men :Testosterone.
- In female : Estrogen replacement therapy e. g. .clomiphene, ofimoxifene.
- 1,000 mg of calcium for those aged 19–50, and 1,200 mg for those aged 50 and above.
- Capsules or sachets 1,000 IU once a week for 8 weeks ,than one daily.
- Oral or IV. In Post Menopausal osteoporosis. Dose once monthly oral and quarterly IV. Once monthly dose is associated with good safety and tolerability.
- Every three to four weeks 4 mg infusion.
- Miacalcic nasal spray : One puff daily for 3-6 weeks, gives good pain relief for spinal compression osteoporotic fracture.
9 . Protein food supplements
- 1 tablespoon thrice a day (may be mixed with milk or a beverage}.
- Spinal extension exercises.
- Use of spinal support.
- High protein diet.
- To refrain from bending the back and lifting weight.
- Avoid Corticosteroid drugs
- Non weight bearing crutch walking.
- Calcitriol 0.5 mg daily prevents loss of bones in patient starting treatment with steroids.
- Calcium by mouth.
- Estrogen replacement in pos menopausal women.
- Calcitonin nasal spray one puff daily for one month.
- Physiotherapy, Exercises
- Vitamins & Calcium supplement- Calcium 1.5 to 2 grams per day
- Vitamin D3 Vitamin D is commonly known as the “sunshine vitamin.” That’s because your skin makes vitamin D when it is exposed to sunlight

- If calcium malabsorption cholecalciferol 0.25 mg (10,000) IU
- Estrogen therapy for small thin women or early menopause
- Calcitonin also inhibits bone reabsorption and has been shown to prevent menopausal bone loss.
- Bisphosphate inhibit bone reabsorption
- Sodium fluoride stimulates osteoblasts and new bone formation
- Estrogen replacement in postmenopausal women
People with osteoporosis are at higher risk of falls due to poor postural control, muscle weakness, and overall deconditioning. Postural control is important to maintaining functional movements such as walking and standing. Physical therapy may be an effective way to address postural weakness that may result from vertebral fractures, which are common in people with osteoporosis. Physical therapy treatment plans for people with vertebral fractures include balance training, postural correction, trunk and lower extremity muscle strengthening exercises, and moderate-intensity aerobic physical activity. The goal of these interventions are to regain normal spine curvatures, increase spine stability, and improve functional performance. Physical therapy interventions were also designed to slow the rate of bone loss through home exercise programs.
 |
| Hip protectors |
Hip protectors decrease the number of hip fractures among the elderly. They are cost effective More modern hip protectors do not suffer from these disadvantages because they are slimmer with a low profile, so less noticeable, have ventilation holes and ducting to keep the skin cool under the pad and are soft and pliable conforming to the contours of the hip. Types : Hip protectors are either of the "crash helmet type" or "energy-absorbing type". The "crash helmet type" distributes impacts into the surrounding soft tissue, while the "energy-absorbing type" is made of a compressible material and diminishes the force of impact. Both of these systems aim to reduce the focused force beneath an estimated fracture threshold.
- Abhyanga Massage with Sesame or til / mustard oil daily for strengthening the bones
- Panchkarma treatment that involves snehana (oleation), swedana (sudation), and mild purifying therapies
- Intake of foods, which are of sweet, sour and salt taste
- Gandha tailam- taken orally as well as for local application
- Asthisamharaka :A Panacea for bone health. Name : Cissus quadrangilaris, hadjod, (joining bone) devil's backbone, or adamant creeper or bone vine, miracle healer. Vajra balli, Mangara balli, Pirandai, KandvelIt is a potential and effective bone builder supplement. In pregnancy it is consumed for bone health. Tablets are made from it. used for joint injury, broken bone care and healing ligament properties. It is used for fixing bone fracture. Stem paste mixing with egg albumin and applied on the affected part. By boiling its leaves and stems, a curry is prepared to consume, which is believed to cure osteoarthritis.
It has hot potency which alleviates Vata and kapha dosha. It posses dry light and mild laxative attributes. It is an appetizer, digestant, an aphrodisiac and a bone healer. Uses : Rich in calcium, it is advised to use during pregnancy, child birth and for weakness due to menopause ( or menorrhagia)To treat bone fractures, the crushed stems are used as a poultice over bone fracture, A medicated ghee is prepared and administered orally. To get rid of obesity, diabetes, heart problem, cancer and in metabolic syndrome. Asthisamharaka is also prescribed as a general tonic.



.jpg)





.png)






.jpg)




.png)


.jpg)



.jpg)








.jpeg)


























.jpg)



.jpg)











.webp)














Great info
ReplyDeleteThanks.
ReplyDeleteedirne
ReplyDeletetrabzon
adana
yozgat
V6UZ