Esophageal Varices
Esophageal Varices
(Esophageal varix, Cirrhosis, Hepatic Dis function,Portal Hypertension, End stage liver disease.)
 |
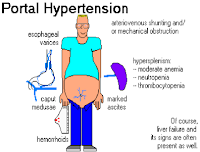
| Portal Hypertension |
Esophageal varices are abnormal, enlarged veins in the tube that connects the throat and stomach (esophagus) . This condition occurs most often in people with serious liver diseases.
Esophageal varices develop when normal blood flow to the liver is blocked by a clot or scar tissue in the liver. To go around the blockages, blood flow around the smaller blood vessels that aren't designed to carry large volumes of blood. The vessels can leak blood or even rupture, causing life threatening bleeding.
Number of drugs and medical procedures can help prevent and stop bleeding from esophageal varices.
There are more than 1 million cases per year of esophageal varices. It is treatable by medical professionals. Requires a medical diagnosis. Lab test or imaging always required. Chronic can last for years or be lifelong.
At the time of diagnosis, approximately 30% of cirrhotic patients have esophageal varices, reaching 90% after approximately 10 years. Bleeding from esophageal varices is associated with a mortality of at least 20% at 6 weeks, although bleeding ceases spontaneously in up to 40% of patients. Variceal hemorrhage is the most common fatal complication of cirrhosis.
Introduction
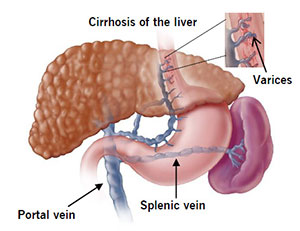
The esophagus (food pipe) is the tube that connects your throat to your stomach. Esophageal varices are enlarged veins in the esophagus in people with cirrhosis of the liver.. They're often due to obstructed blood flow through the portal vein, which carries blood from the intestine, pancreas and spleen to the liver. These veins may rupture and bleed.
Esophageal varices usually develop when blood flow to the liver is blocked. They often occur in people with advanced liver disease.Usually there are no symptoms unless the veins bleed.
"People with esophageal varices have a strong tendency to develop severe bleeding which left untreated can be fatal."
 |
| Esophageal Varices with prominent Red Cherry Spot |
"Consult a specialist in Gastroenterology, Hematology and Hepatology (Liver Disease)"
Pathogenesis
The upper two thirds of the esophagus are drained via the esophageal veins, which carry deoxygenated blood from the esophagus to the azygos vein, which in turn drains directly into the superior vena cava . These veins have no part in the development of esophageal varices. The lower one third of the esophagus is drained into the superficial veins lining the esophageal mucosa, which drain into the left gastric vein, which in turn drains directly into the portal vein. These superficial veins (normally only approximately 1 mm in diameter) become distended up to 1–2 cm in diameter in association with portal hypertension.
Normal portal pressure is approximately 9 mm Hg compared to an inferior vena cava pressure of 2–6 mm Hg. This creates a normal pressure gradient of 3–7 mm Hg. If the portal pressure rises above 12 mm Hg, this gradient rises to 7–10 mm Hg.[5] A gradient greater than 5 mm Hg is considered portal hypertension. At gradients greater than 10 mm Hg, blood flowing through the hepatic portal system is redirected from the liver into areas with lower venous pressures. This means that collateral circulation develops in the lower esophagus, abdominal wall, stomach, and rectum. The small blood vessels in these areas become distended, becoming more thin-walled, and appear as varocosities.
In situations where portal pressures increase, such as with cirrhosis, there is dilation of veins in the anastomosis, leading to esophageal varices. Splenic vein thrombosis is a rare condition that causes esophageal varices without a raised portal pressure. Splenectomy can cure the variceal bleeding due to splenic vein thrombosis
Varices can also form in other areas of the body, including the stomach (gastric varices), duodenum (duodenal varices), and rectum (rectal varices).
Treatment of these types of varices may differ. In some cases, schistosomiasis also leads to esophageal varices
In situations where portal pressures increase, such as with cirrhosis, there is dilation of veins in the anastomosis, leading to esophageal varices. Splenic vein thrombosis is a rare condition that causes esophageal varices without a raised portal pressure. Splenectomy can cure the variceal bleeding due to splenic vein thrombosis
Varices can also form in other areas of the body, including the stomach (gastric varices), duodenum (duodenal varices), and rectum (rectal varices).
Treatment of these types of varices may differ. In some cases, schistosomiasis also leads to esophageal varices
Grading of Varices
- Grade 1 : Small straight esophageal varices.
- Grade 2 : Enlarged, tortuous esophageal varices occupying less than 1/3rd of the lumen.
- Grade 3 : Large, coil shaped esophageal varices occupying more than 1/3rd of the lumen.
Histology
Dilated sub-mucosal veins are the most prominent histologic feature of esophageal varices. The expansion of the sub-mucosa leads to elevation of the mucosa above the surrounding tissue, which is apparent during endoscopy and is a key diagnostic feature. Evidence of recent variceal hemorrhage includes necrosis and ulceration. Evidence of past variceal hemorrhage includes inflammation and venous thrombosis.
Causes
- Cirrhosis of liver (scarring) is the most common cause of esophageal varices. This scarring cuts down on blood flowing through the liver. As a result, more blood flows through the veins of the esophagus.The extra blood flow causes the veins in the esophagus to balloon outward. Heavy bleeding can occur if the veins tear.
- Chronic liver disease : Any type of long-term (chronic) liver disease can cause esophageal varices. Varices can also occur in the upper part of the stomach.
- Hepatitis
- Portal Hypertension (High blood pressure in portal vein) and the associated blood vessels in the hepatic or liver based. or liver based circulation.
- Alcoholism :
- Schistosomiasis also leads to esophageal varices. disease caused by parasitic flatworms.
- Splenic vein thrombosis :
Signs & Symptoms
Chronic Liver disease
- Pallor
- Edema :
- Finger Clubbing :
- Pruritis : Scratch marks.
- Chronic Fatigue :
- Abdominal Pain :
- Diarrhea :
- Fever :
- Weight loss
- Leuconykia : (Hypoalbuminemia)
- Muscle Wasting
- Palmer Errythema : (Impaired breakdown of sex hormones) Palmer erythema is a skin condition that makes the palms of your hands turn red. It can be hereditary but can also be the result of a variety of health conditions (Fatty liver disease.) . Palmer erythema is also known as liver palms, red palms, or Lane's disease.
- Dupuytren's Contracture
- Decreased body hair:
- Parotid enlargement :
- Testicular Atrophy :
- Xanthelasmia :
- Esophageal Varices
 |
| Esophageal Varices |
- Vomiting Blood / Hematemesis
 |
| Hematemesis |
- Ascitis : Ascitis is the main complication of cirrhosis, and the mean time period to its development is approximately 10 years. Ascitis is a landmark in the progression into the decompensated phase of cirrhosis and is associated with a poor prognosis and quality of life; mortality is estimated to be 50% in 2 years.
- Caput medusae is the name for a cluster of swollen veins in your abdomen. (Dilated veins around the umbilicus due to portal hypertension) The swelling usually appears around the belly button, and the veins branch out from a central point. They are typically painless, but they are a symptom of circulatory problems that are often related to liver disease
- Ascitis
- Cirrhosis of liver : Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as hepatitis and chronic alcoholism. Each time your liver is injured — whether by disease, excessive alcohol consumption or another cause — it tries to repair itself.
- Hepatmegaly : Hepatomegaly is an enlarged liver, which means it's swollen beyond its usual size
- Anemia
- Ankle edema
- Coma
- Shock
- Scleral Icterus / Jaundice : (Increased bilirubin due to dysfunction of metabolism) yellowish pigmentation of the skin, tissues, and body fluids caused by the deposition of bile pigments
- Bleeding tendencies (Decrease Prothrombin)
- Passing Black stool / Malena tar-like or bloody stools and, in severe cases.
- Dark urine colour :
- Ecchymosis : (Defective coagulation) : It is the discolouration of skin caused by extravasation of blood due to the rupture of underlying capillaries that leads to collection of blood outside the cells.
- Bruising :
- Asterixis : Liver Flap / Course Tremors (Abnormal motor act due to faulty mechanism)
- Fetor hepaticus (Breath smells like a freshly opened corpse) occurs when your breath has a strong, musty smell. It's a sign that your liver is having trouble doing its job of filtering out toxic substances, usually due to severe liver disease. As a result, sulfur substances end up in your bloodstream and can make their way to your lungs.
- Gynacomastia : (Impaired breakdown of estrogen ) Gynecomastia is a condition of over development or enlargement of the breast tissue in men or boys
Diagnosis
Detection of esophageal varices in liver cirrhosis
Elastography
An elastography, also known as liver elastography, is a type of imaging test that checks the liver for fibrosis. Fibrosis is a condition that reduces blood flow to and inside the liver. This causes the buildup of scar tissue. Left untreated, fibrosis can lead to serious problems in the liver.
Liver Elastography
Transient Elastography (Fibro Scan)
Acoustic Radiation force impulse Imaging
Shear Wave Elastography
Spleen Elastography
Imaging Technique
Computed Tomography (C.T Scan)
Magnetic resonance Imaging (M.R.I)
Ultrasound
Laboratory Examination
Spleen Platelet Count
Spleen diameter ratio
Blood Test
- Blood Test Complete blood count Hemoglobin, reduced platelet count.
- Liver function Test : Bilirubin
- Prothrombin time (bleeding time & clotting time.)
- Hypoalbuminemia
- Urine test R.B.C in urine + bilirubin
Capsule Endoscopy
Grade Endoscopic finding
0 Absence of esophageal varices.
1 Micro-vessels that sketch varicose strings located in the esophagogastric transition or in the distal esophagus.
2 One or two fine caliber varices (smaller than 3 mm diameter) located in the distal esophagus.
3 Medium caliber varices (between 3 or 6 mm diameter) or more than varices up to 3 mm that may reach up to a third medium third of the esophagus.
4 Thick caliber varices, larger than 6 mm diameter, in any part of esophagus.
Hepatic venous pressure gradient (H.V.P.G)
Measurement is the best available method to evaluate the presence and severity of portal hypertension. Clinically significant portal hypertension is defined as an increase in H.V.P.G to >10 mm Hg
- Currently, no treatment can prevent the development of esophageal varices in people with liver disease.
- While beta blockers drugs are effective in preventing bleeding in many people who have esophageal varices, they do not keep esophageal varices from forming.
- If one have been diagnosed with liver disease, strategies to avoid liver disease complications should be taken.
- Don't drink alcohol.
- Eat a healthy diet.
- Reduce your risk of hepatitis.
Treatments include beta blockers, medical procedures to stop bleeding, and in rare cases, liver transplant.
Emergency
- Resuscitate and provide intravenous volume support and blood transfusion (caution there is a risk of over transfusion)
- Carry out balloon tamponade - e.g with a Sengstaken tube- even if endoscope facilities are not available for diagnosing varices.
- Transfer the patient to the nearest district hospital with endoscopy facilities.
- Carry our endoscopy and Sclerotherapy.
- The cheapest agent is ethanolamine oleate, which can be prepared in the hospital pharmacy.
- Propranolol (for life) and iron therapy as needed.
- Band ligators vary in price, the cheapest method is probably to reload the rubber ligators for reuse.
- Histoacryl is the preferred product in many African countries.Cheap products are available from India where sterile sesame oil is used instead of Liliodol.
Treatment
In emergency situations, care is directed at :
- Stopping blood loss,
- Maintaining plasma volume,
- Correcting disorders in coagulation induced by cirrhosis
- Appropriate use of antibiotics such as quinolones or ceftriaxone .
- Blood volume resuscitation should be done promptly and with caution. The goal should be hemodynamic stability and hemoglobin of over 8 g/dl. Resuscitation of all lost blood leads to increase in portal pressure leading to more bleeding. Volume resuscitation can also worsen ascites and increase portal pressure. (A.A.S.L.D guidelines)
- Therapeutic Endoscopy is considered the mainstay of urgent treatment. The two main therapeutic approaches are
- Variceal ligation (Banding ) and Sclerotherapy
- In cases of refractory bleeding, balloon tamponade with a Sengstaken-Blakemore tube may be necessary, usually as a bridge to further endoscopy or treatment of the underlying cause of bleeding (i.e: portal hypertension).
- Esophageal de-vascularization operations such as the Sugiura procedure can also be used to stop complicated bleeding. Methods of treating the portal hypertension include: trans jugular intrahepatic portosystemic shunt (TIPS), distal splenorenal shunt procedure, or liver transplantation.
- Nutritional supplementation is necessary if the person has been unable to eat for more than four days.
- Terlipressin and octreotide for one to five days have also been used.
Nurse to monitor
- Assess for alcohol use.
- Monitor electrolytes
- Instruct client on foods to avoid. (Spicy)
- Priority for blood transfusion.
- Central line & Pulmonary artery pressures.
- Blood transfusions & fresh frozen plasma for clotting factors.
- Somatostatin or Vasopressin - constrict gut vessels.
- Airways.
Later prevention of Re-bleeding
- Beta Blockers
- Long acting nitrates.
- Soft foods, chew well, avoid Intra-abdominal pressure.(avoid constipation,coughing)
- Protonix.(Pantoprazole is used to treat certain stomach and esophagus problems (such as acid reflux). It works by decreasing the amount of acid your stomach makes.)
Beta blocker drugs
The non-selective Beta-blockers (e.g., Propranolol, timolol,or nadolol)
Non-selective beta blockers (but not cardio selective beta blockers like Atenelol ) are preferred because they decrease both cardiac output by β1 blockade and splanchnic blood flow by blocking vasodilating β2 receptors at splanchnic vasculature.
However, non-selective beta blockers do not prevent the formation of esophageal varices.
When medical contraindications to beta-blockers exist, such as significant reactive airway disease, then treatment with prophylactic endoscopic variceal ligation is often performed
Long acting Nitrates
(e.g., Isosorbide mono nitrate (I.M.N) have been evaluated for secondary prophylaxis.
Treatments include beta blockers, medical procedures to stop bleeding, and in rare cases, liver transplant.
Endoscopic ligature esophageal varices banding Rubber band ligation.
Endoscopic Variceal Ligation
Ligation of esophageal varices
Banding of esophageal Varices
Endoscopic Variceal ligation
Endoscopic Band Ligation
Complication
- Internal Bleeding
- Hypovolemic shock
- Cardiac arrest.
The most serious complication of esophageal varices is bleeding. Once you have had a bleeding episode your risk of having another episode greatly increases.If you lose enough blood,you can go into shock,which can lead to death.
https://madhuchhandacdmo.blogspot.com/2022/01/bleeding-esophageal-varices.html










































.jpeg)
Comments
Post a Comment