Hyponatremia / Low salt level
Hyponatremia / Low salt level
A normal blood sodium level is between 135 and 145 milliequivalents per liter (mEq/L). Hyponatremia occurs when the sodium in your blood falls below 135 mEq/L.
Hyponatremia results from the inability of the kidney to excrete a water load or excess water intake.Water intake depends upon thirst mechanism.Thirst is stimulated by increase in osmolality.Thirst is sensed by osmoreceptors located in the hypothalamus and leads to the release of anti-diuretic hormone (vasopressin) from the posterior pituitary.
"To salt or not to salt?—That is the question in cirrhosis".
Introduction
Hyponetremia is a lower than normal level of sodium in the blood stream. It is low concentration of sodium in blood.
Hyponatremia is a condition that occurs when the level of sodium in your blood is abnormally low. Sodium is an electrolyte, and it helps regulate the amount of water that's in and around your cells.In hyponatremia, body's water levels rise, and cells begin to swell. This swelling can cause many health problems, from mild to life-threatening.
"Hyponatremia represents a relative excess of water in relation to sodium."
"Hyponatremia represents a relative excess of water in relation to sodium."
Ascites is the most common complication of patients with cirrhosis, resulting from portal hypertension and vasodilatation. It is associated with an increased risk for the development of hyponatremia and renal failure and has a high mortality rate of 20% per year. The development of ascites represents a baleful sign in the course of disease in cirrhosis. To prevent complications of cirrhosis and improve quality of life, an effective management of ascites is pivotal. Combined salt restriction and diuretic therapy is recommended as first-line therapy in numerous clinical practice guidelines. In contrast, there has been a debate on whether a strict salt-restricted diet for cirrhosis patients should be used at all since salt restriction may increase the risk for malnutrition which in turn may negatively impact on quality of life and survival. This review aims to summarize the current pros and cons regarding salt restriction in patients with cirrhosis and proposes the importance of achieving a sodium balance throughout different stages of cirrhosis.
"Personalized salt management, based on the individual sodium balance of the patient, with regular re-evaluation of sodium and fluid status seems to be necessary."
Water shifts from the intracellular to the extracellular compartment, with a resultant dilution of sodium.
Hypervolemic hyponatremia
Greatly increased total body water, normal total body sodium. Symptoms: edema.It is seen in congestive heart failure and cirrhosis of liver, nephrotic syndrome and chronic kidney disease.Even though the plasma and extracellular volumes is increased in heart failure and cirrhosis, there is ADH stimulation. Total body sodium increases, and TBW increases to a greater extent.Can be renal or non-renalacute or chronic renal failuredysfunctional kidneys are unable to excrete the excess ingested water load (and sodium).
Greatly increased total body water, normal total body sodium. Symptoms: edema.It is seen in congestive heart failure and cirrhosis of liver, nephrotic syndrome and chronic kidney disease.Even though the plasma and extracellular volumes is increased in heart failure and cirrhosis, there is ADH stimulation. Total body sodium increases, and TBW increases to a greater extent.Can be renal or non-renalacute or chronic renal failuredysfunctional kidneys are unable to excrete the excess ingested water load (and sodium).
A condition that occurs when the level of sodium in the blood is too low.
With this condition, the body holds onto too much water. This dilutes the amount of sodium in the blood and causes levels to be low.
Types
- Low volume :Low volume hyponatremia can occur from diarrhea, vomiting, diuretics, and sweating
- Normal volume : Normal volume hyponatremia is divided into cases with dilute urine and concentrated urine. Cases in which the urine is dilute include adrenal insufficiency, hypothyroidism, and drinking too much water or too much beer. Cases in which the urine is concentrated include syndrome of inappropriate antidiuretic hormone secretion.
- High volume : High volume hyponatremia can occur from heart failure, liver failure, and kidney failure. Conditions that can lead to falsely low sodium measurements include high blood protein levels such as in multiple myeloma, high blood fat levels and high blood sugar level.
Diagnostic
- Serum sodium < 135 mmol/L
- Assessments of alertness, concentration, and orientation.
Cause
High volume :
- Cirrhosis of the liver
- Congestive heart failure
- Nephrotic syndrome in the kidneys
- Excessive drinking of fluids
Low volume
Hypovolemia (extracellular volume loss) is due to total body sodium loss. Hyponatremia is caused by a relatively smaller loss in total body water.
- Any cause of hypovolemia such as prolonged vomiting, decreased oral intake, severe diarrhea
- Diuretic use (due to the diuretic causing a volume depleted state and thence ADH release, and not a direct result of diuretic-induced urine sodium loss)
- Addison's disease and congenital adrenal hyperplasia in which the adrenal glands do not produce enough steroid hormones (combined glucocorticoid and mineralocorticoid deficiency)
- Pancreatitis
- Prolonged exercise and sweating, combined with drinking water without electrolytes is the cause of exercise associated Hyponetremia (EAH). It is common in marathon runners and participants of other endurance events.
- The use of MDMA (ecstasy) can result in hyponatremia.
Normal volume
There is volume expansion in the body, no edema, but hyponatremia occurs.
- SIADH (and its many causes)
- Hypothyroidism
- Not enough ACTH
- Beer potomania
- Normal physiologic change of pregnancy
- Reset osmostat
Medication
Antipsychotics have been reported to cause hyponatremia i
Available evidence suggests that all classes of psychotropics, i.e., antidepressants, antipsychotics, , mood stabilizers, and sedative/ hypnotics can lead to hyponatremia. Age is a significant factor for drug induced hyponatremia
- False or pseudo hyponatremia is caused by a false lab measurement of sodium due to massive increases in blood triglyceride levels or extreme elevation of immunoglobulins as may occur in multiple myeloma.
- Hyponatremia with elevated tonicity can occur with high blood sugar, causing a shift of excess free water into the serum.
- Alcohol consumption can be one contributing factor to hyponatremia.
- Hepatic cirrhosis
- Cardiac
- Renal
- Pulmonary Disease :pneumonia, TB
- Medications : Antipsychotic
- Cerebral Diseases :Temporal arteritis, meningitis (meninges is the membrane around brain and spinal cord), encephalitis
- Healthy one can have hyponatremia only due to excess of water intake compareto water excreted
- Hypovolemic hyponatremia
Non-renal lossGastro-Intestinal lossesVomiting, Diarrhea, fistulas, pancreatitisExcessive sweatingCerebral/Renal salt-wasting syndrome (C/RSW)traumatic brain injury, and intracranial surgeryMust distinguish from SIADH (syndrome of the inappropriate antidiuretic Hormones) encountered in infections, malignancy, chest diseases, trauma, surgery etc. - Iso/Euvolemic hyponatremia
Exercise-associated Euvolemic hyponatremiaMarathon runners may develop severe hyponatremia due to excessive water intake associated with persistent ADH secretion in some.Low dietary solute intakeBeer drinkers or other malnourished patients (those with low-protein, high water intake diets) have a marked reduction in water excretory capacity despite suppressed ADH.Infants who may have been given inappropriate amounts of free waterbowel preparation before colonoscopy or colorectal surgery
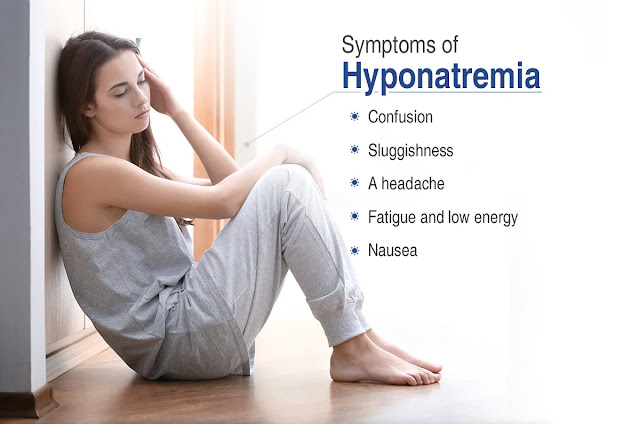
Symptoms
- Nausea and vomiting.
- Headache.
- Confusion.
- Loss of energy, drowsiness and fatigue.
- Restlessness and irritability.
- Muscle weakness, spasms or cramps.
- Seizures.
- Coma.
- Cerebral Oedema : is excess accumulation of fluid in the intra/extracellular spaces of the brain.
"Hyponatremia represents a relative excess of water in relation to sodium."
EpidemiologyAcute hyponatremia (developing rapidly, in 48 h or less) are subject to more severe degrees of cerebral edema, brain swelling and can lead to comaCerebral edema or cerebral oedema is excess accumulation of fluid in the intra/extracellular spaces of the brain. Chronic hyponatremia (developing gradually, in days or weeks) experience milder degrees of cerebral edemaBrainstem herniation has not been observed in patients with chronic hyponatremia
"Sodium level is less than 105 mmol/L, the mortality is over 50%"
Physiology Serum sodium concentration regulation:
- Stimulation of thirst
- Secretion of ADH which is also called arginine vasopressin. It’s a hormone made by the hypothalamus in the brain and stored in the posterior Pituitary gland. It tells your kidneys how much water to conserve.
- Renal handling of filtered sodium
- Osmolality increases
- Main driving force
- Only requires an increase of 2 - 3%
- Blood volume or pressure is reduced
- Requires a decrease of %
- Thirst center is located in the anterio-lateral center of the hypothalamus
- Respond to NaCl and angiotensin II
Hyponatremia Pathophysiology
- Hyponatremia can only occur when some condition impairs normal free water excretion
- Acute drop in the serum osmolality
- Neuronal cell swelling occurs due to the water shift from the extracellular space to the intracellular space
- Swelling of the brain cells elicits 2 responses for osmoregulation, as follows:
- It inhibits ADH secretion and hypothalamic thirst center
- Immediate cellular adaptation
Treatment
Limited fluid intake, medication and hospitalization may be required
Fluids and proteins are typically the cornerstone of initial management.
Treatment is based on the underlying cause. Correcting hyponatremia too quickly can lead to complications.
- Rapid partial correction with 3% Normal Saline is only recommended in those with significant symptoms.
- Low volume hyponatremia is typically treated with intravenous normal saline.
- Syndrome of inappropriate antidiuretic hormone secretion (SIADH) is typically treated by correcting the underlying cause and with fluid restrictions.
- While high volume hyponatremia is typically treated with both fluid restriction and a diet low in salt. Correction should generally be gradual in those in whom the low levels have been present for more than two days.
Hyponatremia is the most common type of electrolyte imbalance, and is often found in older adults. It occurs in about 20% of those admitted to hospital and 10% of people during or after an endurance sporting event. Among those in hospital, hyponatremia is associated with an increased risk of death.
Vasopressin receptor antagonist (vaptans), such as conivaptin may be slightly more effective than fluid restriction in those with high volume or normal volume hyponatremia.
Daily use of urea by mouth, while not commonly used due to the taste, has tentative evidence in SIADH
People who have hyponatremia who require hospitalization have a longer length of stay (with associated increased costs) and also have a higher likelihood of requiring readmission. This is particularly the case in men and in the elderly
https://madhuchhandacdmo.blogspot.com/2022/12/hyponatremia-low-salt-level.html 

.jpeg)
Comments
Post a Comment